| 〔Case Report〕 |
| Carcinoma in adenoma of the duodenal bulb accompanied by gastrointestinal stromal tumor (GIST) of the stomach
|
|
| Norikazu Kuroiwa1), Kenji Oda1), Keiji Koda2) Kazuhiro Seike3), Takashi Nikaido4) and Masaru Miyazaki1)
|
| (Received February 2, 2006, Accepted February 24, 2006) |
|
SUMMARY
Primary carcinoma of the duodenal bulb is very rare. We report herein on a case involving a patient with early duodenal bulb carcinoma accompanied by gastrointestinal stromal tumor (GIST) of the stomach. A 74-year-old woman was found by computed tomography (CT) to have a gastric submucosal tumor. Endoscopic examination revealed a submucosal tumor of the stomach, and a large, superficially elevated lesion at the duodenal bulb. Gastric wedge resection and distal gastrectomy were performed. Reconstruction was carried out according to the Billroth II method. Histologically, the submucosal tumor was diagnosed as gastrointestinal stromal tumor (GIST), and the duodenal tumor was diagnosed as well-differentiated tubular adenocarcinoma in tubulo-villous adenoma. The patient recovered uneventfully, and was healthy, having had no recurrence, 3 years and 6 months after surgery. To the best of our knowledge, the superficially elevated bulb carcinoma in our case may be larger than any other previously reported ones.
|
|
Key Words
| Duodenal carcinoma, Carcinoma in adenoma, Gastric GIST |
|
| |
Ⅰ.Introduction
Early duodenal carcinoma occurs far less frequently than other gastrointestinal malignancies. The first reported case of primary duodenal carcinoma was described by Hamburger in 1746. From then, 694 cases had been presented in the literature up to 1974. Recently, progress in gastroduodenal endoscopy has enabled early detection of duodenal carcinoma. In this paper, we report a case of early duodenal carcinoma accompanied by gastrointestinal stromal tumor (GIST) of the stomach.
Ⅱ.Case
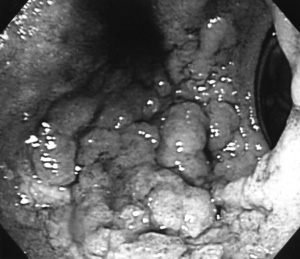
A 74-year-old woman, who had previously undergone thyroid tumor extirpation in 1981 and extended thymectomy in April 2002, was found by abdominal computed tomography (CT) in follow-up studies to have a solid tumor attached to the posterior wall of the gastric corpus. It was diagnosed as gastric submucosal tumor (SMT) by upper gastrointestinal series and gastroduodenal endoscopy. Moreover, a large, superficially elevated lesion was detected at the duodenal bulb (Fig. 1). Biopsy specimens of this duodenal tumor revealed well-differentiated tubular adenocarcinoma.
The patient was admitted to our department on June 21, 2002. Laboratory data showed mild anemia (Hb 10.7 g/dl), but other data were normal, including tumor markers (CEA 2.1 ng/ml, CA19-9 5.1 U/ml).
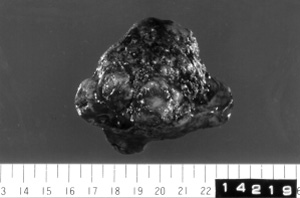
Surgery was performed on July 2, 2002. An egg-sized, hard tumor was located at the dorsal side of upper corpus of the stomach. Gastric wedge resection was performed (Fig. 2). Distal gastrectomy was also performed to remove the duodenal carcinoma. During operation, endoscopy was used in determining the duodenal cutting line, and frozen section revealed no carcinoma cells at the distal margin. Reconstruction was carried out according to the Billroth II method.
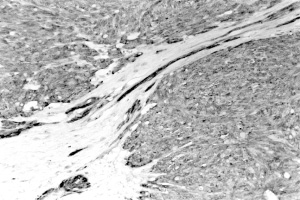
Histologically, the submucosal tumor consisted of spindle-shaped cells with oval nuclei, and there were very few mitoses. Immunostaining showed the reactibility of tumor cells to the c-kit (Fig. 3), CD34, Vimentin, but not with SMA, Desmin, NSE, S-100 protein. The tumor was categorized as a gastrointestinal stromal tumor (GIST), of the uncommitted type.
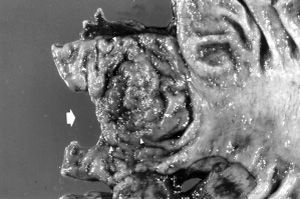
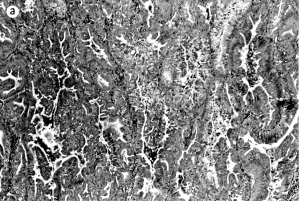
The duodenal tumor was 50 x 50 mm in size, soft, granular, and superficially elevated (Fig. 4). Microscopically, it was composed of well-differentiated tubular adenocarcinoma and tubulo-villous adenoma with moderate to severe atypia (Fig. 5a, 5b). The depth of tumor invasion was restricted to the mucosal layer.
The patient recovered uneventfully, and was healthy, having had no recurrence, 3 years and 6 months after surgery.
|
 |
 |
| Fig. 1 Endoscopic view of the duodenal tumor. The tumor is large, superficially elevated and occupy |
Fig. 2 Resected specimen of the gastric submucosal tumor. The tumor shows extraluminal growth.
|
|
 |
 |
| Fig. 3 The tumor cells are immunoreactive to c-kit. x 230. |
Fig. 4 Gross finding of the duodenal tumor. The tumor is granular and superficially elevated (arrowhead). The distal margin was examined by frozen section (arrow).
|
|
 |
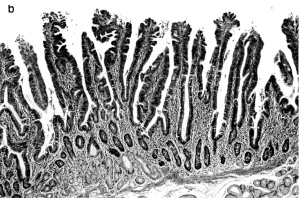 |
| Fig. 5 Microscopic findings of the duodenal tumor. a Well-differentiated tubular adenocarcinoma. Hematoxylin and eosin. x 100. b Tubulo-villous adenoma with moderate to severe atypia. Hematoxylin and eosin. x 65. |
|
Ⅲ.Discussion
Primary duodenal carcinomas other than Vater papilla carcinoma are very rare. Kleinerman et al.[1]reported that its incidence was 0.035% of autopsy cases. It is estimated that duodenal carcinoma represents 0.35% of all gastrointestinal carcinomas[2], and 33% to 45% of all small intestinal carcinomas[1,2].
The distribution of primary duodenal carcinoma, reported in the literatures is 23%-26% supurapapillary, 48%-59% peripapillary, and 18%-26% infrapapillary[1,2]. However, in 1999, Arai et al.[3]indicated a proximal shift in duodenal carcinoma among elderly patients. In our case, the patient was 74 years old. The proximal duodenum is reportedly the most common site of carcinogenesis[3].
The histogenesis of primary duodenal carcinoma has been categorized as: (1) de novo carcinogenesis (49%), (2) adenoma-carcinoma sequence (42%), (3) transformation from Brunner’s gland (6%), (4) transformation from heterogenic gastric mucosa (3%)[4]. In our case, duodenal tumor was 50 x 50 mm in size, and was composed of well-differentiated tubular adenocarcinoma and tubulo-villous adenoma. The proportion of underlying villous adenoma seemed to be higher than previously reported, and that suggested an adenoma-carcinoma sequence[5,6].
About 40% of patients with early duodenal carcinoma have no complaint[4]. Recently, many cases seem to be unexpectedly detected during examinations of other preceding lesions, or during screening. Careful observation of the duodenum is required during endoscopic examination.
In the present case, duodenal bulb resection was performed with distal gastrectomy, because of the large size of the duodenal tumor. Intraoperative endoscopy and frozen section examination were of great help in determining the distal margin. Some authors have reported successful results of endoscopic treatment for early, small duodenal carcinomas[7,8].
The patient in the present case suffered from thyroid adenoma, thymoma, duodenal carcinoma and gastric GIST. We were not able to determine their relationship with each other. No specific family history was identified. The causes of metachronous and synchronous tumor multiplicity are still unknown. Ho et al.[9]reported a case of primary duodenal carcinoma and small bowel leiomyomas in a patient with neurofibromatosis. To the best of our knowledge, the superficially elevated bulb carcinoma in our case may be larger than any other previously reported ones (PubMed, until January 2006, key word: duodenal bulb cancer).
|
|
要旨
| 我々は,高機能自閉症患者が視線弁別の際に「心の理論theory of mind (ToM)」に関連する脳部位の異常活性を認めるかについて検証した。磁気共鳴機能画像法functional Magnetic Resonance Imagingを用いて,5人の高機能自閉症患者と9人の健常者に視線弁別のタスクを行なった。この結果,健常者では患者群に比べて,左中前頭回,右頭頂間溝,両側中心前回,両側下頭頂回により高い活性が認められた。一方,患者群では健常者に比べて左上側頭回,右島,右内側前頭葉により高活性が認められた。以上より,高機能自閉症患者では,(1) ToM関連の脳部位における機能的以上,および (2) 通常,他者の視線からの情報を処理する際には見られない,脳の広範囲にわたる脳部位における機能的異常があることが示唆された。 |
|
References
1) Kleinerman J, Yardumian K, Tamaki HT. Primary carcinoma of duodenum. Ann Intern Med 1950; 32: 451-65.
2) Iovine VM, Tsangaris N. Primary carcinoma of the duodenum. Am Surg 1961; 27: 744-50.
3) Arai T, Murata T, Sawabe M, Takubo K, Esaki Y. Primary adenocarcinoma of the duodenum in the elderly: Clinicopathological and immunohistochemical study of 17 cases. Pathol Int 1999; 49: 23-9. [full text]
4) Fujisawa T, Tomofuji Y, Kuroda N, Hagino H, Sakamoto N, Sakashita M, Maeda M, Kouno T, Matsuno Y. A case of early duodenal cancer with tubulo-villous adenoma: Report of a case and clinico-pathological review of Japanese literature (in Japanese with English abstract). Gastroenterol Endosc 1995: 37: 2768-75.
5) Lai EC, Doty JE, Irving C, Tompkins RK. Primary adenocarcinoma of the duodenum: Analysis of survival. World J Surg 1988; 12: 695-9.
6) Scott-Coombes DM, Williamson RCN. Surgical treatment of primary duodenal carcinoma: A personal series. Br J Surg 1994; 18: 1472-4.[PubMed]
7) Tringali M, Crotta S, Bodrato C, Lolli R, Cerrato C, Cerrato G. Early primary duodenal carcinoma successfully treated by endoscopic polypectomy. Endoscopy 1994; 26: 709.
8) Terai K, Gonda H, Fujii Y, Seki E, Sekine Y, Matsuoka T, Daibo M, Sakurai H, Tamura T, Saito H. A case of early duodenal cancer resected by endoscopic mucosal resection (in Japanese with English abstract). Prog Digest Endosc 2001; 59: 96-7.
9) Ho KT, Tan KA, Gwee HM, Lee SK, Foog WC. A case of primary duodenal carcinoma and small bowel leiomyomas in a patient with neurofibromatosis. Sing Med J 1980; 21: 713-6.
|
|
Others
1)Department of General Surgery and 2)Department of Frontier Surgery, Graduate School of Medicine, Chiba University, Chiba 260-8670.
3)Department of Surgery, Odawara Municipal Hospital, Kanagawa 250-8558.
4)Department of Pathology, Jikei University School of Medicine, Tokyo 105-8471.
黒岩教和1),小田健司1),幸田圭史2),清家和裕3),二階堂隆4),宮 勝1): 胃GISTを併発した十二指腸球部腺腫内癌の1例.
1)千葉大学大学院医学研究院臓器制御外科学
2)千葉大学大学院医学研究院先端応用外科学
3)小田原市立病院外科
4)東京慈恵会医科大学病理部
Tel. 043-222-7171. Fax. 043-226-2552. e-mail: odaken-cib@umin.ac.jp
2006年2月2日受付,2006年2月24日受理.
|
|
|
|
|
|
|
|
|
|